Sudden Cardiac Death And Sports

Introduction
In 2016, the Summer Olympic Games were held in Brazil, and the European Football Championship in France. These quadrennial events, with attendant huge media coverage, bring into focus the considerable international fascination with competitive sports. Participating athletes in such events as well as sports participants in general are usually healthy and are perceived to be fit. It is also accepted that regular sports activity is beneficial in reducing long-term overall as well as cardiovascular mortality, including sudden cardiac death (SCD).[1–7] However, the occasional instance of SCD during a sporting event in full public glare serves as a grim reminder of the small but definite arrhythmic risk of extreme exercise. This paradox of exercise has been described for over 30 years.[2–4]
We need to place into perspective the current thoughts on screening and other measures to improve outcomes.
Sports Activity: Conclusively Beneficial for Long-term Sudden Cardiac Death Risk
Cardiovascular advantages of physical activity are well-established, and the excessive attention often focused on sports-SCD should not overshadow the broad issue that regular exercise has irrefutable benefits.[8] Several studies have established that regular physical activity is associated with lower long-term risk of SCD.[7,9–12] There is scientific consensus that a certain amount of physical activity is strongly recommended to reduce overall mortality,[13] including SCD. On the other hand, for sports-SCD, an analogy of 'drug overdosage'[14] has been used, considering that sports (exercise) is in fact an effective 'drug' for SCD risk reduction. This analogy suggests that the association between sports and mortality may follow a U-curve;[15] moderate sports would confer a lower overall mortality, whereas strenuous sports activity would be associated with a similar mortality as a non-exercising population due to a counterbalancing effect of short-term SCD risk. However, this concept remains controversial.
Sudden Death in the Young Competitive Athlete: Tip of the Iceberg
A 'young competitive athlete' is traditionally defined as any person 10–35 years old who participates in an organized sports program (team or individual sport) that requires regular competition and training.[16–19] SCD occurring among young competitive athletes has always attracted major media attention, with emblematic examples in footballers[20] or, more recently, cyclists.[21] To date, the large majority of data on sports-SCD have focused on the burden among young competitive athletes, and the extent to which intensive physical activity may be actually harmful. However, sudden death in competitive athletes is a very low-frequency event.[22,23] While accurate estimation of the incidence of sports-SCD among young competitive athletes is challenging, it is estimated to be less than 10 per million per year in a recent meta-analysis.[23] By contrast, considering the burden of sports participation in the general population, focusing on competitive athletes alone could lead to a rather biased perspective on sports-SCD.
Sudden Cardiac Death Among Recreational Sports Participants: The Majority of Sports-sudden Cardiac Death
Sports-SCD accounts for a small but significant proportion of all SCD, with recent studies consistently reporting around 5% of overall SCD occurring during sporting activity.[24,25] It may be estimated that sports-SCD likely accounts for 15 000 cases annually in North America and in Europe. This estimate underlines the important magnitude of this entity. Literature on sports-SCD, during recreational sports activities in the community, remains relatively sparse. The emphasis on young competitive athletes as opposed to recreational sports participants is discordant with the relative magnitudes of the respective problems, which was recently highlighted by a population-based registry.[17] Overall, among all sports-SCD, only 6% occurred in young competitive athletes, as compared with 94% among recreational sports participants (Figure 1).[17] This is intuitive given the large pool of recreational sports participants as compared to competitive athletes. Thus, there is a crucial need to focus attention on this large at-risk population of subjects.
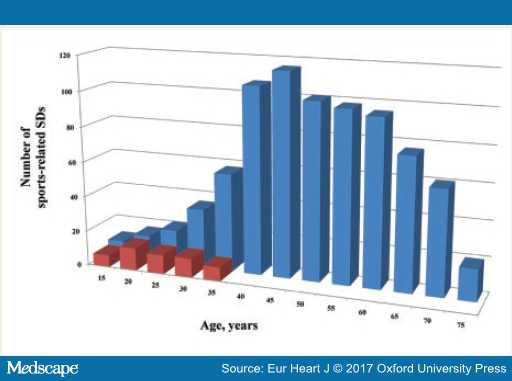
Figure 1. Distribution by age of sports-sudden cardiac death in young competitive athlete (red) and general population (blue) (From Ref 17).
Sports-sudden Cardiac Death Presents With Highly Homogenous Characteristics
Results from three large population-based registries published recently have elucidated the fairly uniform characteristics of sports-SCD.[17,24,25] This form of SCD usually afflicts middle-aged patients, with a striking male predominance (>90% of cases). In terms of medical history, a significant fraction of patients had previous heart disease,[17,24] and interestingly, several patients presented with symptoms (chest pain, dyspnoea) during the week before sports-SCD,[24] which were usually neglected. Attention to this could potentially create room for subacute prevention, with better identification of high-risk patients and education for self-assessment of risk.
Regarding circumstances, most sports-SCD occurred in public places,[26] and a large majority of cases (around 90%) were bystander-witnessed, often with multiple witnesses. This almost-universal presence of a bystander permits precise phenotyping of sports-SCD, with precise information on presentation and delays (including time from collapse to CPR). Rates of bystander-CPR were substantially higher than those described in the non-sport setting, from 30 to 80%, and an initial shockable rhythm was found in 50–80% of cases (as compared to three—four fold lower in non-sports setting[27,28]). Due to the above mentioned characteristics, survival is notably higher in sports-SCD, ranging from 16 to 45% in multiple international reports,[17,25] compared to less than 10% for overall SCD.[28,29]
How to Tackle Sports-sudden Cardiac Death?
Strategies to reduce the burden of sports-SCD can be considered under two approaches, namely, primary prevention (through pre-participation screening and population education) and improved management of the SCD event (to increase survival rate). These approaches should ideally complement each other to achieve best results.
Primary prevention of sports-SCD relies on pre-participation screening of sports participants, as well as education of participants and other stakeholders in sporting events. Considering that most of these events are due to cardiovascular diseases, there is an ongoing controversy regarding the delivery of pre-participation screening and early identification of asymptomatic structural or electrical abnormalities in this population, with postulated benefits[16] but uncertainty regarding cost-effectiveness.[30] A seemingly attractive and logical way for prevention would be to screen patients for asymptomatic cardiac lesions before sports participation.
To this end, an understanding of the usual underlying causes of sports-SCD is crucial. Under 30 years of age, the main causes are inheritable diseases such as hypertrophic cardiomyopathy and arrhythmogenic right ventricular cardiomyopathy. Over 30 years, atherosclerotic coronary disease strongly prevails. Guidelines regarding cardiovascular evaluation before sports activity[31] suggest that to assess sport-SCD risk among middle age sport participants, the main issues to consider are medical history, level of physical activity and previous exercise training. To further enhance screening, especially among young competitive athletes, strategies based on systematic performance of 12-lead ECG have been proposed.[16,32] While this has had some promising results, there is significant ongoing controversy about such an approach with regard to cost-effectiveness, false positive rates and the potential psychological impact on a young target population.[30,33] Notwithstanding these features, considering the potential benefits, current guidelines advocate pre-participation ECG screening.[34] While governmental legislation has even been considered with regard to sports participation,[35] this debate has often been emotionally fraught and is a difficult dilemma for clinicians. A universal and undifferentiated strategy of screening is probably not an effective approach. However, identification of select subgroups that might benefit from such screening remains problematic. One would need to start with certain broad areas of focus such as among middle-aged men, where, considering the higher risk, effective ways to enhance pre-participation screening need to be actively sought. Considering the recent data that previous warning symptoms were present in several instances of sports-SCD,[24] systematic assessment of such symptoms, and education of participants to identify them and take appropriate action, appears necessary.
SCD occurring during sports activity offers a particularly suitable setting to achieve a favourable outcome that needs to be capitalized upon. However, one needs to bear in mind that this overall picture often masks major regional disparities in survival across regions, varying, for instance, from less than 10 to almost 50% (Figure 2) in France.[36] This heterogeneity in survival rates is similar to results from studies performed in overall SCD.[37] However, in contrast to all SCD occurring in the general population, sport-SCD almost universally presents with homogenous characteristics as pointed out earlier.[36] Therefore, the specific setting of sports-SCD offers a unique opportunity to better analyse the key determinants of survival in SCD (Figure 3). Interestingly, bystander CPR appears as one of the main prognostic factors, a result highly consistent in recent reports.[29]
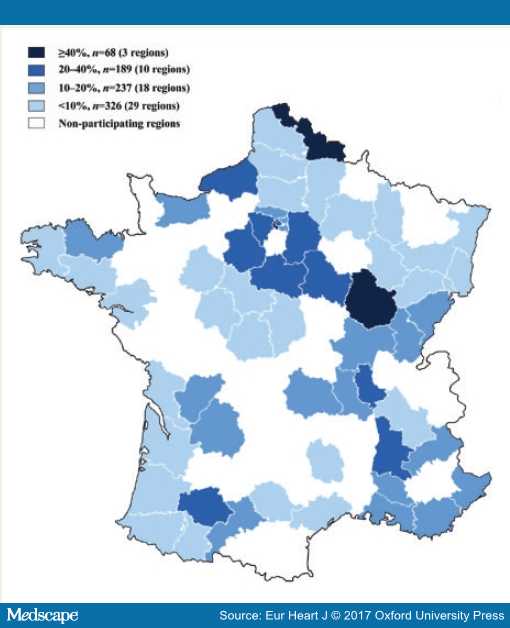
Figure 2. Survival rates after sport-sudden cardiac death across districts in France (From Ref 36).
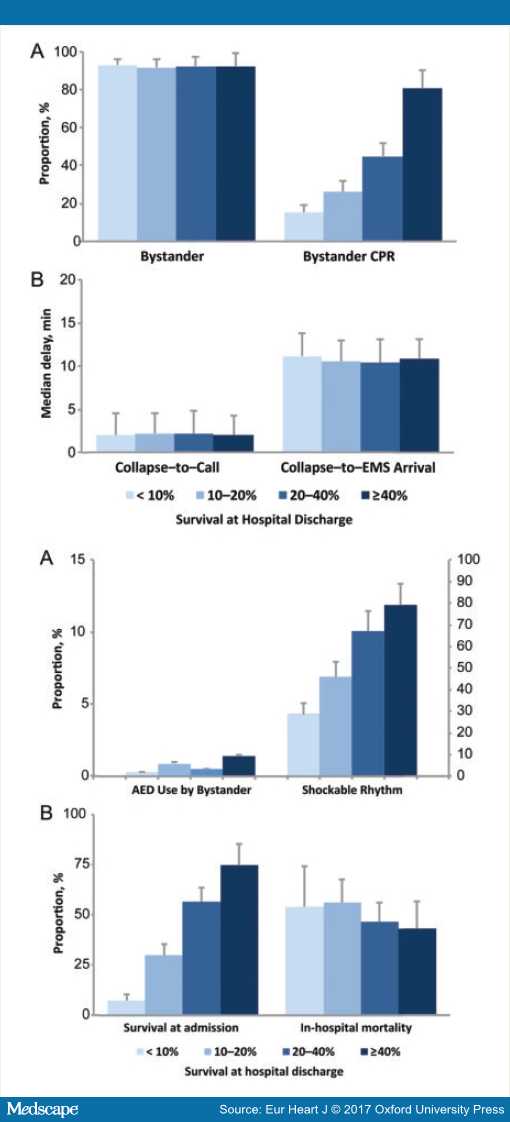
Figure 3. Factors associated with rates of survival at hospital discharge after sport-sudden cardiac death (From Ref 36).
Finally, sports-SCD could be considered as a 'quasi-experimental' situation to demonstrate the potential benefit of a particular intervention in a relatively controlled environment, as previously described for implementation of public-access defibrillation (in sports facilities[38–40]). Widespread deployment of Automatic External Defibrillators (AEDs) in sport facilities, for example, may be a major tool available to enhance survival in sports-SCD.[38,39] To this end, recent guidelines advocated that AEDs should be widely distributed throughout the arena or on mobile emergency responders to achieve the goal of first defibrillation within 5 min of a witnessed collapse.[39] Thus, while survival in sports-SCD is better than for all SCD, room for improvement clearly remains in the form of public education, improved bystander CPR rates, and better AED access.
Conclusion
Though the specific entity of sports-SCD is often a devastating and emotionally charged event in a young individual, exercise in general, is clearly beneficial and has a role in the prevention and therapy of cardiac disease, indeed even in long-term prevention of sports-SCD. Therefore, the goal for healthcare providers should certainly not be to discourage sports participation. However, there should be concerted efforts to enhance prevention and management of sports-SCD, which appears to be a particularly suitable model for specific therapies. Targeted prevention through tailored and individualized pre-participation screening and an enhanced focus on middle-aged men during recreational sports could be of particular benefit.
References
- Sharma S, Merghani A, Mont L. Exercise and the heart: the good, the bad, and the ugly. Eur Heart J 2015;36:1445–1453.
- Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med 1984;311:874–877.
- Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med 2000;343:1355–1361.
- Maron BJ. The paradox of exercise. N Engl J Med 2000;343:1409–1411.
- Lee D-C, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol 2014;64:472–481.
- Conraads VM, Beckers P, Vaes J, Martin M, Van Hoof V, De Maeyer C, Possemiers N, Wuyts FL, Vrints CJ. Combined endurance/resistance training reduces NT-proBNP levels in patients with chronic heart failure. Eur Heart J 2004;25:1797–1805.
- Whang W, Manson JE, Hu FB, Chae CU, Rexrode KM, Willett WC, Stampfer MJ, Albert CM. Physical exertion, exercise, and sudden cardiac death in women. JAMA 2006;295:1399–1403.
- Arena R, Guazzi M, Lianov L, Whitsel L, Berra K, Lavie CJ, Kaminsky L, Williams M, Hivert M-F, Cherie Franklin N, Myers J, Dengel D, Lloyd-Jones DM, Pinto FJ, Cosentino F, Halle M, Gielen S, Dendale P, Niebauer J, Pelliccia A, Giannuzzi P, Corra U, Piepoli MF, Guthrie G, Shurney D, AHA Writing Group, Arena R, Berra K, Dengel D, Franklin NC, et al. Healthy lifestyle interventions to combat noncommunicable disease-a novel nonhierarchical connectivity model for key stakeholders: a policy statement from the American Heart Association, European Society of Cardiology, European Association for Cardiovascular Prevention and Rehabilitation, and American College of Preventive Medicine. Eur Heart J 2015;36:2097–2109.
- Chiuve SE, Fung TT, Rexrode KM, Spiegelman D, Manson JE, Stampfer MJ, Albert CM. Adherence to a low-risk, healthy lifestyle and risk of sudden cardiac death among women. JAMA 2011;306:62–69.
- Deo R, Vittinghoff E, Lin F, Tseng ZH, Hulley SB, Shlipak MG. Risk factor and prediction modeling for sudden cardiac death in women with coronary artery disease. Arch Intern Med 2011;171:1703–1709.
- Deo R, Albert CM. Epidemiology and genetics of sudden cardiac death. Circulation 2012;125:620–637.
- Wannamethee G, Shaper AG, Macfarlane PW, Walker M. Risk factors for sudden cardiac death in middle-aged British men. Circulation 1995;91:1749–1756.
- Wen CP, Wai JPM, Tsai MK, Yang YC, Cheng TYD, Lee M-C, Chan HT, Tsao CK, Tsai SP, Wu X. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011;378:1244–1253.
- O'Keefe JH, Lavie CJ. Run for your life … at a comfortable speed and not too far. Heart 2013;99:516–519.
- Schnohr P, O'Keefe JH, Marott JL, Lange P, Jensen GB. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol 2015;65:411–419.
- Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006;296:1593–1601.
- Marijon E, Tafflet M, Celermajer DS, Dumas F, Perier M-C, Mustafic H, Toussaint J-F, Desnos M, Rieu M, Benameur N, Le Heuzey J-Y, Empana J-P, Jouven X. Sports-related sudden death in the general population. Circulation 2011;124:672–681.
- Pelliccia A, Di Paolo FM, Corrado D, Buccolieri C, Quattrini FM, Pisicchio C, Spataro A, Biffi A, Granata M, Maron BJ. Evidence for efficacy of the Italian national pre-participation screening programme for identification of hypertrophic cardiomyopathy in competitive athletes. Eur Heart J 2006;27:2196–2200.
- Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol 2003;42:1959–1963.
- Dvorak J. A lion never dies: pro memoria of Marc-Vivien Foé. Br J Sports Med 2009;43:628.
- Daan Myngheer: Cycling mourns second Belgian death. BBC Sport. http://www.bbc.com/sport/cycling/35914893 (1 April 2016)
- Kim JH, Malhotra R, Chiampas G, Hemecourt P d', Troyanos C, Cianca J, Smith RN, Wang TJ, Roberts WO, Thompson PD, Baggish AL. Cardiac arrest during long-distance running races. N Engl J Med 2012;366:130–140.
- Gerardin B, Collet J-P, Mustafic H, Bellemain-Appaix A, Benamer H, Monsegu J, Teiger E, Livarek B, Jaffry M, Lamhaut L, Fleischel C, Aubry P, Groupe de Réflexion sur la Cardiologie Interventionnelle. Registry on acute cardiovascular events during endurance running races: the prospective RACE Paris registry. Eur Heart J 2015;
- Marijon E, Uy-Evanado A, Reinier K, Teodorescu C, Narayanan K, Jouven X, Gunson K, Jui J, Chugh SS. Sudden Cardiac Arrest During Sports Activity in Middle Age. Circulation 2015;131:1384–1391.
- Berdowski J, Beus MF de, Blom M, Bardai A, Bots ML, Doevendans PA, Grobbee DE, Tan HL, Tijssen JGP, Koster RW, Mosterd A. Exercise-related out-of-hospital cardiac arrest in the general population: incidence and prognosis. Eur Heart J 2013;34:3616–3623.
- Marijon E, Bougouin W, Karam N, Beganton F, Lamhaut L, Perier M-C, Benameur N, Tafflet M, Beal G, Hagege A, Le Heuzey J-Y, Desnos M, Spaulding C, Carré F, Dumas F, Celermajer DS, Cariou A, Jouven X. Survival from sports-related sudden cardiac arrest: In sports facilities versus outside of sports facilities. Am Heart J 2015;170:339–345.e1.
- Rea TD, Eisenberg MS, Becker LJ, Murray JA, Hearne T. Temporal trends in sudden cardiac arrest: a 25-year emergency medical services perspective. Circulation 2003;107:2780–2785.
- Bougouin W, Lamhaut L, Marijon E, Jost D, Dumas F, Deye N, Beganton F, Empana J-P, Chazelle E, Cariou A, Jouven X. Characteristics and prognosis of sudden cardiac death in Greater Paris : Population-based approach from the Paris Sudden Death Expertise Center (Paris-SDEC). Intensive Care Med 2014;40:846–854.
- Hasselqvist-Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out-ofhospital cardiac arrest. N Engl J Med 2015;372:2307–2315.
- Halkin A, Steinvil A, Rosso R, Adler A, Rozovski U, Viskin S. Preventing sudden death of athletes with electrocardiographic screening: what is the absolute benefit and how much will it cost? J Am Coll Cardiol 2012;60:2271–2276.
- Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, Halle M, Heidbüchel H, Björnstad HH, Gielen S, Mezzani A, Corrado D, Pelliccia A, Vanhees L. Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 2011;18:446–458.
- Corrado D, Pelliccia A, Bjørnstad HH, Vanhees L, Biffi A, Borjesson M, Panhuyzen-Goedkoop N, Deligiannis A, Solberg E, Dugmore D, Mellwig KP, Assanelli D, Delise P, Buuren F van-, Anastasakis A, Heidbuchel H, Hoffmann E, Fagard R, Priori SG, Basso C, Arbustini E, Blomstrom-Lundqvist C, McKenna WJ, Thiene G, Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 2005;26:516–524.
- Wheeler MT, Heidenreich PA, Froelicher VF, Hlatky MA, Ashley EA. Cost-effectiveness of preparticipation screening for prevention of sudden cardiac death in young athletes. Ann Intern Med 2010;152:276–286.
- Corrado D, Schmied C, Basso C, Borjesson M, Schiavon M, Pelliccia A, Vanhees L, Thiene G. Risk of sports: do we need a pre-participation screening for competitive and leisure athletes? Eur Heart J 2011;32:934–944.
- http://www.nasbe.org/healthy_schools/hs/bytopics.php?topicid=2190.
- Marijon E, Bougouin W, Celermajer DS, Perier M-C, Benameur N, Lamhaut L, Karam N, Dumas F, Tafflet M, Prugger C, Mustafic H, Rifler J-P, Desnos M, Le Heuzey J-Y, Spaulding CM, Avillach P, Cariou A, Empana J-P, Jouven X. Major regional disparities in outcomes after sudden cardiac arrest during sports. Eur Heart J 2013;34:3632–3640.
- Girotra S, Diepen S van, Nallamothu BK, Carrel M, Vellano K, Anderson ML, McNally B, Abella B, Sasson C, Chan PS, in collaboration with CARES Surveillance Group and the Heart Rescue Project. Regional Variation in Out-of-Hospital Cardiac Arrest Survival in the United States. Circulation 2016;
- Borjesson M, Dugmore D, Mellwig K-P, Buuren F van, Serratosa L, Solberg EE, Pelliccia A, Rehabilitation on behalf of the SCS of the EA of CP and, Cardiology ES of. Time for action regarding cardiovascular emergency care at sports arenas: a lesson from the Arena study. European Heart Journal 2010;31:1438–1441.
- Borjesson M, Serratosa L, Carre F, Corrado D, Drezner J, Dugmore DL, Heidbuchel HH, Mellwig K-P, Panhuyzen-Goedkoop NM, Papadakis M, Rasmusen H, Sharma S, Solberg EE, Buuren F van, Pelliccia A, writing group on behalf of the EACPR Section of Sports Cardiology. Consensus document regarding cardiovascular safety at sports arenas: position stand from the European Association of Cardiovascular Prevention and Rehabilitation (EACPR), section of Sports Cardiology. Eur Heart J 2011;32:2119–2124.
- Page RL, Husain S, White LY, Rea TD, Fahrenbruch C, Yin L, Kudenchuk PJ, Cobb LA, Eisenberg MS. Cardiac arrest at exercise facilities: implications for placement of automated external defibrillators. J Am Coll Cardiol 2013;62:2102–2109.
- Lebreton G, Pozzi M, Luyt C-E, Chastre J, Carli P, Pavie A, Leprince P, Vivien B. Out-of-hospital extra-corporeal life support implantation during refractory cardiac arrest in a half-marathon runner. Resuscitation 2011;82:1239–1242.
Story Credit: http://www.medscape.com/viewarticle/880591_1


